Drug information
| drug-audio-en-Tucidinostat.mp3 |
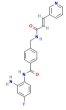
C22 H19 F N4 O2
N-(2-amino-4-fluorophenyl)-4-[[[(E)-3-pyridin-3-ylprop-2-enoyl]amino]methyl]benzamide
Tucidinostat is in Phase 2/3 development as a latency-reversing agent for HIV.
(Compound details obtained from PubChem,1 HUYA Bioscience International website,2 and Treatment Action Group website3)
Pharmacology
Mechanism of Action
Latency-reversing agent, specifically a histone deacetylase inhibitor (HDACi).3 Tucidinostat, a benzamide derivative, is an HDACi that selectively targets the class I HDAC enzymes HDAC-1, -2, and -3, which are important in the disruption of HIV latency. Additionally, tucidinostat is active against the class II HDAC-10 enzyme.4,5 Tucidinostat has also been shown to reactivate latent HIV via the NF-κB signaling pathway.6 Currently, tucidinostat is approved for use in China and Japan for the treatment of certain types of cancer.7
In HIV-1 latency, HDACs are recruited to the proviral 5' long terminal repeat (LTR), where they catalyze deacetylation of lysine residues on histones, resulting in chromatin condensation on nucleosome 1 (nuc-1) and preventing HIV transcription. Inhibition of HDAC activity promotes histone acetylation (hyperacetylation) of lysine residues by histone acetyltransferases (HATs), leading to chromatin relaxation and transcriptional activation.5,8 Some research suggests that the activity of HDACis in inducing HIV transcription may not be caused by direct effects on histone acetylation, but may be caused by effects on other non-histone proteins.9,10
Half-life (T1/2)
In a Phase 1b/2a trial (NCT02513901) evaluating tucidinostat in adults with HIV, the elimination half-life of tucidinostat after a single oral 10-mg dose was approximately 11.5 hours. After multiple oral 10-mg doses of tucidinostat, the half-life was approximately 15.5 hours.11
Select Clinical Trials
Study Identifiers: CHARTER; NCT02513901
Sponsor: Tang-Du Hospital
Phase: 1b/2a
Status: This study has been completed.
Study Purpose: The purpose of this open-label trial was to evaluate the safety of tucidinostat plus ART and the efficacy of tucidinostat plus ART in reactivating HIV transcription in latently infected cells and reducing latent HIV reservoir size.
Study Population:
- Participants were adults with HIV who were on ART and who had been receiving ART for at least 18 months.
- Participants had HIV RNA <50 copies/mL for at least 1 year and had CD4 counts >350 cells/mm3.11,12
Selected Study Results: Results presented at AIDS 2018 and published in the journal HIV Medicine (2020) showed that tucidinostat added to ART in seven participants with viral suppression robustly reactivated latent HIV and modestly reduced the latent HIV reservoir size.11,13
Study Identifier: NCT02902185
Sponsor: Tang-Du Hospital
Phase: 2/3
Status: This study has been completed.
Study Purpose: The purpose of this study was to confirm the efficacy of tucidinostat plus ART in reactivating HIV transcription in latently infected cells and reducing latent HIV reservoir size.
Study Population:
- Participants were adults with HIV who were on ART and who had been receiving ART for at least 24 months.
- Participants had HIV RNA <20 copies/mL for at least 1.5 years and had CD4 counts >350 cells/mm3.3,14
Study Identifier: NCT04985890
Sponsor: UBP Greater China (Shanghai) Co., Ltd
Phase: 2
Status: See the ClinicalTrials.gov record for this study's status.
Study Purpose: The purpose of this open-label study is to evaluate the safety of tucidinostat plus the CD4 attachment inhibitor semzuvolimab (UB-421) and the ability of this regimen in reducing the HIV reservoir in participants undergoing an analytical treatment interruption of ART.
Study Population:
- Participants are adults with HIV who have been receiving ART for more than 1 year and who have more than two different alternative optimized ART regimens available.
- Participants have had HIV RNA <50 copies/mL for at least 12 months prior to screening.15
Study Identifier: NCT05056974
Sponsor: United BioPharma
Phase: 2
Status: This study has been completed.
Study Purpose: The purpose of this open-label study was to assess the safety and efficacy of tucidinostat plus semzuvolimab (UB-421) monotherapy in changing the latent HIV reservoir in participants who underwent an analytical treatment interruption of ART.
Study Population:
- Participants were adults with HIV who were on ART for more than 3 years.
- Participants had stable viral suppression.16
Study Identifier: NCT05129189
Sponsor: Shanghai Public Health Clinical Center
Phase: 2
Status: This study is currently recruiting participants.
Study Purpose: The purpose of this open-label study is to evaluate whether ASC22 (an investigational PD-L1 antibody) combined with tucidinostat can reduce latent HIV reservoir size.
Study Population:
- Participants are adults with HIV who have been receiving ART for at least 24 months.
- Participants had had HIV RNA <50 copies/mL (measured on two consecutive occasions at least 12 months apart) and have had CD4 counts ≥250 cells/mm3 and CD4/CD8 ratios <0.9 during the screening period.17
Selected Study Results: Results presented at IAS 2023 showed that ASC22 combined with tucidinostat activated latent HIV and reduced the size of the latent HIV reservoir only in participants with enhanced T-cell function.18
In addition, a Phase 1 study (NCT03980691) evaluated whether tucidinostat used in combination with chimeric antigen receptor (CAR)-T or T cell receptor (TCR)-T cell therapy could reduce the size of the latent HIV reservoir in participants on suppressive ART. This study has been completed.19
Adverse Events
CHARTER (NCT02513901)
In this Phase 1b/2a trial, seven participants completed treatment with eight oral doses of tucidinostat. No significant adverse events (AEs) occurred, and all AEs were of Grade 1 severity. Rash and fatigue/somnolence were each reported in one participant. A small decrease in complete blood cell counts, most notably red blood cell counts and hemoglobin values, were seen with tucidinostat treatment, but these cases were all below Grade 1 and returned to baseline levels by Day 56. CD4 counts remained unchanged throughout the study.11,20
NCT05129189
In this Phase 2 study, 15 participants were enrolled to receive subcutaneous ASC22 once every 4 weeks for three cycles and oral tucidinostat twice weekly over 12 weeks while maintaining ART. ASC22 and tucidinostat were well tolerated. Nine drug-related AEs were reported, all of which were mild and resolved without treatment.18
Drug Interactions
Information about drug-drug interactions between tucidinostat and HIV-related drugs is currently unavailable.
References
- National Center for Biotechnology Information. PubChem compound summary for CID 12136798, tucidinostat. Accessed January 30, 2024
- Huya Bioscience International: Press Release, dated March 6, 2007. HUYA Bioscience licenses chidamide cancer compound from Chipscreen Biosciences. Accessed January 30, 2024
- Treatment Action Group website. Research toward a cure trials. Accessed January 30, 2024
- Lu X, Ning Z, Li Z, Cao H, Wang X. Development of chidamide for peripheral T-cell lymphoma, the first orphan drug approved in China. Intractable Rare Dis Res. 2016;5(3):185-191. doi:10.5582/irdr.2016.01024. Accessed January 30, 2024
- Matalon S, Rasmussen TA, Dinarello CA. Histone deacetylase inhibitors for purging HIV-1 from the latent reservoir. Mol Med. 2011;17(5-6):466-472. doi:10.2119/molmed.2011.00076. Accessed January 30, 2024
- Yang W, Sun Z, Hua C, et al. Chidamide, a histone deacetylase inhibitor-based anticancer drug, effectively reactivates latent HIV-1 provirus. Microbes Infect. 2018;20(9-10):626-634. doi:10.1016/j.micinf.2017.10.003. Accessed January 30, 2024
- Chipscreen Biosciences. Chidamide. Accessed January 30, 2024
- Rasmussen TA, Tolstrup M, Winckelmann A, Østergaard L, Søgaard OS. Eliminating the latent HIV reservoir by reactivation strategies. Hum Vaccin Immunother. 2013;9(4):790-799. Accessed January 30, 2024
- Shirakawa K, Chavez L, Hakre S, Calvanese V, Verdin E. Reactivation of latent HIV by histone deacetylase inhibitors. Trends Microbiol. 2013;21(6):277-285. doi:10.1016/j.tim.2013.02.005. Accessed January 30, 2024
- Elliott JH, Wightman F, Solomon A, et al. Activation of HIV transcription with short-course vorinostat in HIV-infected patients on suppressive antiretroviral therapy. PLoS Pathog. 2014;10(11). doi:10.1371/journal.ppat.1004473. Accessed January 30, 2024
- Sun Y, Li J, Ma C. Chidamide disrupts and reduces HIV-1 latency in patients on suppressive antiretroviral therapy. Slides presented at: International AIDS Conference; July 23-27, 2018; Amsterdam, Netherlands. Accessed January 30, 2024
- Tang-Du Hospital. Safety and efficacy of the histone deacetylase inhibitor chidamide in combination with antiretroviral therapy for eradication of the latent HIV-1 reservoir (CHARTER). In: ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). Registered on July 30, 2015. NLM Identifier: NCT02513901. Accessed January 30, 2024
- Li JH, Ma J, Kang W, et al. The histone deacetylase inhibitor chidamide induces intermittent viraemia in HIV-infected patients on suppressive antiretroviral therapy. HIV Med. 2020;21(11):747-757. doi:10.1111/hiv.13027. Accessed January 30, 2024
- Tang-Du Hospital. Efficacy of the histone deacetylase inhibitor chidamide in combination with antiretroviral therapy for reactivation of the latent HIV-1 reservoir: a randomized controlled clinical trial. In: ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). Registered on September 6, 2016. NLM Identifier: NCT02902185. Accessed January 30, 2024
- UBP Greater China (Shanghai) Co., Ltd. A proof of concept study to evaluate the safety and efficacy of UB-421 in combination with Chidamide for reduction of HIV reservoir as compared to UB-421 alone in ART stabilized HIV-1 patients who undergo ART interruption. In: ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). Registered on July 8, 2021. NLM Identifier: NCT04985890. Accessed January 30, 2024
- United BioPharma. A Phase II proof-of-concept trial to evaluate the safety and efficacy of UB-421 plus Chidamide for the shock-block-kill mechanism in changing HIV reservoirs among ART stabilized HIV-1 patients who undergo ART interruption. In: ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). Registered on August 18, 2021. NLM Identifier: NCT05056974. Accessed January 30, 2024
- Shanghai Public Health Clinical Center. Functional cure study of anti-PD-L1 antibody ASC22 in combination with chidamide. In: ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). Registered on November 15, 2021. NLM Identifier: NCT05129189. Accessed January 30, 2024
- Wu L, Zheng Z, Xun J, et al. Anti-PD-L1 antibody ASC22 in combination with chidamide potentiates HIV latency reversal and immune function from ART-suppressed individuals: a single center, single-arm, phase II study. Poster presented at: IAS Conference on HIV Science; July 23-26, 2023; Brisbane, Australia and Virtual. Poster LBEPB18. Accessed January 30, 2024
- Guangzhou 8th People’s Hospital. Effect of chidamide combined with CAT-T or TCR-T cell therapy on HIV-1 latent reservoir. In: ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). Registered on June 7, 2019. NLM Identifier: NCT03980691. Accessed January 30, 2024
- Sun Y, Li J, Ma J. Chidamide reactivates and diminishes latent HIV-1 DNA in patients on suppressive antiretroviral therapy. Abstract presented at: International AIDS Conference; July 23-27, 2018; Amsterdam, Netherlands. Abstract WEAA0101. Accessed January 30, 2024
Last Reviewed: January 30, 2024